What is hypoglycaemia?

Hypoglycaemia is when blood sugar falls below the normal range
(less than 3.9 mmol/L or 70 mg/dL).
Types of hypoglycaemia
Mild hypoglycaemia
Severe hypoglycaemia
Nocturnal hypoglycaemia
To align hypoglycaemia terminology in clinical trials and encourage appropriate responses in clinical practice, the IHSG has developed the following definitions:1
Level 1
A glucose alert value of 3.9 mmol/L (70 mg/dL) or less. This often doesn’t need to be reported routinely, depending on the purpose of the clinical study.
Level 2
A glucose alert value of <3.0 mmol/L (<54 mg/dL) is sufficiently low and indicates serious, clinically important hypoglycaemia.
Level 3
As defined by the ADA, severe hypoglycaemia indicates severe cognitive impairment requiring external assistance for recovery.
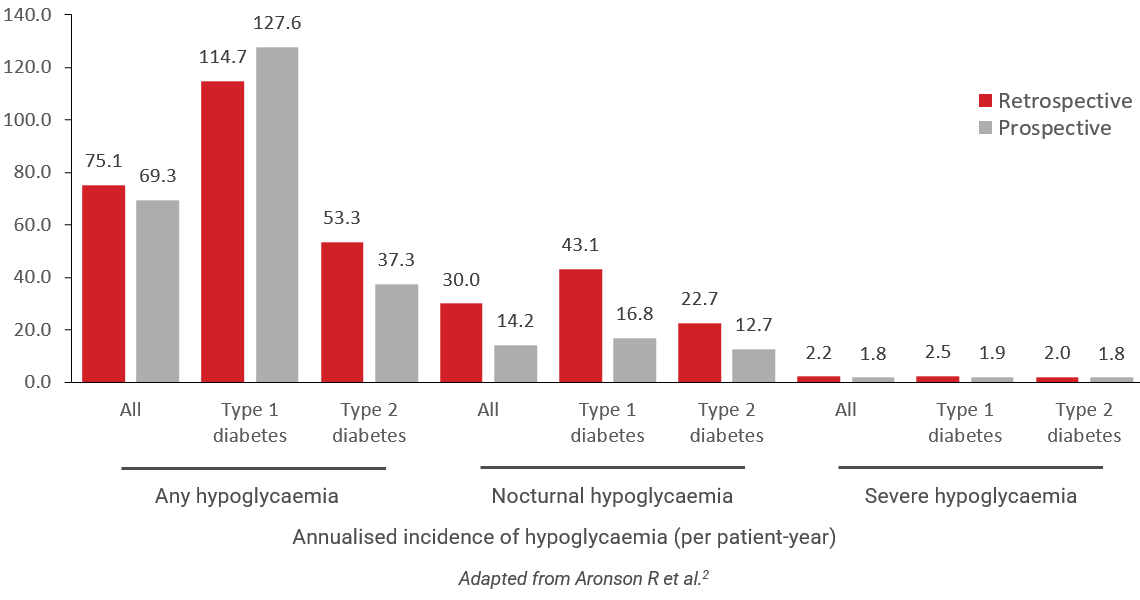
Epidemiology
In people with type 1 diabetes (T1D), for which insulin treatment is assumed, the prevalence of severe hypoglycaemia increases with the duration of T1D.
| Annual prevalence of hypoglycaemia based on T1D duration |
|---|
| People with T1D for less than 5 years 20% develop hypoglycaemia |
| People with T1D for 5 years or more More than 40% develop hypoglycaemia |
| Annual prevalence of hypoglycaemia based on T1D duration | ||
|---|---|---|
| People with T1D for less than 5 years |  |
20% develop hypoglycaemia |
| People with T1D for 5 years or more |  |
More than 40% develop hypoglycaemia |
In people with type 2 diabetes (T2D), both duration and medical treatment influence the risk. The annual risk of severe hypoglycaemia is significant for people with T2D on sulfonylureas (SUs) and on insulin, especially if on insulin for over 5 years (>20% risk). Non-severe hypoglycaemia, which adults can self-treat, is more common than severe hypoglycaemia, but poses far less risk to health and life.
References
- 1International Hypoglycaemia Study Group. Glucose Concentrations of Less Than 3.0 mmol/L (54 mg/dL) Should Be Reported in Clinical Trials: A Joint Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes Diabetes Care 2017;40:155–157.
- 2Aronson R et al. The Canadian Hypoglycemia Assessment Tool Program: Insights Into Rates and Implications of Hypoglycemia From an Observational Study. 2018;42:11–17.
- 3Cryer PE. Elimination of hypoglycemia from the lives of people affected by diabetes. Diabetes 2011;60:24.
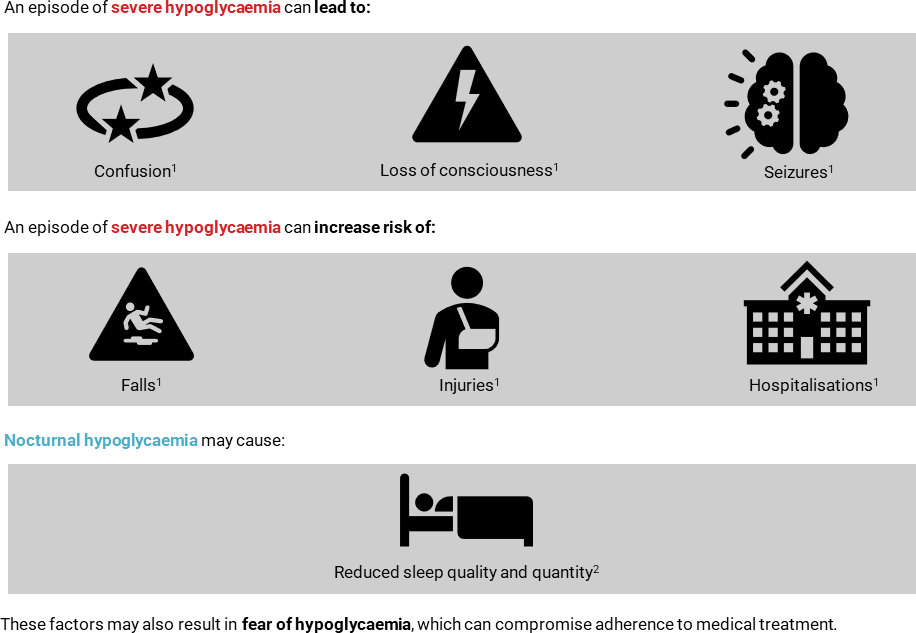
Risks of a hypoglycaemic episode
Episodes of hypoglycaemia can range from uncomfortable to life-threatening.
Long-term clinical impact
People with type 1 diabetes:
|
People with type 2 diabetes:
|
Caregivers:
|
References
- 1Cryer PE. Elimination of hypoglycaemia from the lives of people affected by diabetes. Diabetes 2011;60:24.
- 2
Musen G et al. Impact of Diabetes and Its Treatment on Cognitive Function Among Adolescents Who Participated in the Diabetes Control and Complications Trial. Diabetes Care. 2008; 31:1933–1938.
- 3Kaira SK et al. Hypoglycemia: The neglected complication. Indian J Endocrinol Metab 2013;17:819–834.
- 4Cato A & Hershey T. Cognition and Type 1 Diabetes in Children and Adolescents. Diabetes Spectr 2016;197–202.
- 5Jacobson AM et al. Cognitive performance declines in older adults with type 1 diabetes: results from 32 years of follow-up in the DCCT and EDIC Study. Lancet Diabetes Endocrinol.2021;9:436-445,
- 6Desouza CV et al. Diabetes Care. 2010;1389–1394.
- 7Davis SN et al. Effects of Severe Hypoglycemia on Cardiovascular Outcomes and Death in the Veterans Affairs Diabetes Trial. Diabetes Care 2019;42:157–163.
- 8Hsu PF et al. Association of Clinical Symptomatic Hypoglycemia With Cardiovascular Events and Total Mortality in Type 2 Diabetes. Diabetes Care 2013;36:894–900.
- 9Reifergerste D & Hartleib S. Hypoglycemia-related information seeking among informal caregivers of type 2 diabetes patients: Implications for health education. J Clin Transl Endocrinol. 2016;4:7–12.
Risk factors based on diabetes type1–4
Type 1 diabetes |
|---|
| History of severe episodes |
| HbA1c <6.5% (except in youth) |
| High glucose variability (in older adults) |
| Renal impairment |
| Impaired awareness of hypoglycaemia |
| Advanced age, very young age |
Type 2 diabetes (on insulin or sulfonylureas) |
|---|
| Cognitive impairment |
| Depression |
| Aggressive glycaemia treatment |
| Impaired awareness of hypoglycaemia |
| Duration of insulin therapy |
| Renal impairment and other comorbidities |
| Advanced age |
Factors that may increase risk of nocturnal hypoglycaemia5,6
- Stress
- Diabetic neuropathy
- Physical exercise, especially during the evening
- Excess insulin during the day
- Previous episodes of nocturnal hypoglycaemia
- High dose of basal insulin
- Failure to check blood glucose at bedtime
- Excess rapid-acting insulin to correct high glucose, particularly at bedtime, or to cover bedtime snacks
- Physical exercise, especially during the evening
- Premix or short-acting insulin before dinner
- NPH insulin (isophane) in the evening
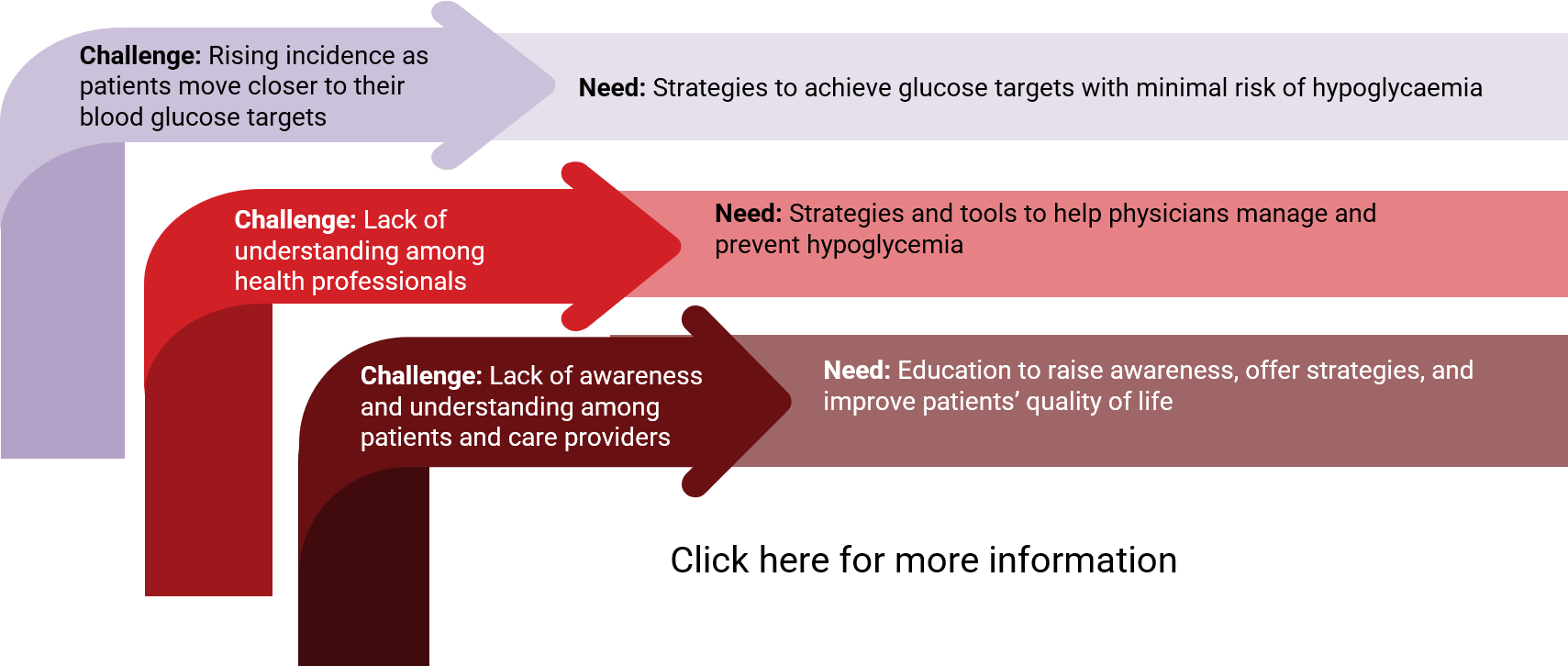
Key needs to mitigate risks
References
- 1Yale JF et al. Hypoglycaemia.
In: Diabetes Canada Full Guidelines.
2018. Available at:
https://guidelines.diabetes.ca/cpg
/chapter14. - 2International Hypoglycaemia Study Group. Minimizing hypoglycaemia in diabetes. Diabetes Care 2015;38:1583.
- 3Inzucchi SE et al. Management of hyperglycemia in Type 2 diabetes, 2015: A patient-centered approach. Diabetes Care 2015;38:
- 4Weinstock RS et al. Risk factors associated with severe hypoglycemia in older adults with Type 1 diabetes. Diabetes Care 2016 Apr;39:603.
- 5Vu L et al. Predicting Nocturnal Hypoglycaemia from Continuous Glucose Monitoring Data with Extended Prediction Horizon. AMIA Annu Symp Proc. 2019;874-882
- 6Brunton SA. Nocturnal hypoglycemia: Answering the challenge with long-acting insulin analogs. MedGenMed 2007;9:38.
- 1Yale JF et al. Hypoglycaemia. In: Diabetes Canada Full Guidelines. 2018. Available at: https://guidelines.diabetes.ca/cpg/chapter14.
- 2International Hypoglycaemia Study Group. Minimizing hypoglycaemia in diabetes. Diabetes Care 2015;38:1583.
- 3Inzucchi SE et al. Management of hyperglycemia in Type 2 diabetes, 2015: A patient-centered approach. Diabetes Care 2015;38:
- 4Weinstock RS et al. Risk factors associated with severe hypoglycemia in older adults with Type 1 diabetes. Diabetes Care 2016 Apr;39:603.
- 5Vu L et al. Predicting Nocturnal Hypoglycaemia from Continuous Glucose Monitoring Data with Extended Prediction Horizon. AMIA Annu Symp Proc. 2019;874-882
- 6Brunton SA. Nocturnal hypoglycemia: Answering the challenge with long-acting insulin analogs. MedGenMed 2007;9:38.
Diagnosis of hypoglycaemia
Hypoglycaemia can be diagnosed clinically and/or biochemically (based on blood glucose levels). Common symptoms of hypoglycaemia include:1,2,3
Autonomic
- Trembling
- Pounding heart
- Sweating
- Anxiety
- Hunger
Neuroglycopenic
- Difficulty concentrating
- Confusion
- Weakness
- Drowsiness, dizziness
- Vision changes
- Difficulty speaking
Nonspecific
- Nausea
- Headache
The IHSG defines blood glucose <3.0 mmol/L (54 mg/dL) as “serious biochemical hypoglycaemia” and
3.5 to 3.9 mmol/L (63 to 70 mmol/L), in the absence of symptoms, as an “alert range”
[See more information here]. People with blood glucose >3.9 mmol/L occasionally report hypoglycaemia symptoms, a presentation that has been described as “pseudohypoglycaemia.”1
References
- 1Edelman SV, Blose JS. the impact of nocturnal hypoglycemia on clinical and cost-related issues in patients with type 1 and type 2 diabetes. Diabetes Educ 2014;40:269.
- 2Graveling AJ, Frier BM. Impaired awareness of hypoglycaemia: a review. Diabetes & Metabolism2010;36: S64.
- 3McAulay V et al. Symptoms of hypoglycemia in people with diabetes. Diabet Med 2001;18:690.
What is impaired awareness of hypoglycaemia?
Impaired awareness of hypoglycaemia (IAH) is the reduced ability to perceive the onset of hypoglycaemia.
How does IAH arise?
IAH arises when repeated episodes of hypoglycaemia raise the glycaemic threshold for symptoms to occur. This means symptoms are only triggered at a lower blood glucose level than normal, causing symptoms not to occur when they should.
Avoidance of hypoglycaemia can reverse IAH2, though this strategy may run the risk of compromising glycaemic control.
Who does IAH affect?
IAH only happens in people regularly taking hypoglycaemic agents such as insulin, and a careful clinical history is often sufficient to identify IAH.2
IAH has varying occurrence by diabetes type:
20-25%
of individuals with
Type 1 diabetes1
10%
of individuals with
Type 2 diabetes1
What are the possible risks of IAH?

References
- 1Van Meijel LA et al. High prevalence of impaired awareness of hypoglycemia and severe hypoglycemia among people with insulin-treated type 2 diabetes: The Dutch Diabetes Pearl CohortBMJ Open Diabetes Res Care 2020;8:e000935.
- 2Farrell CM & McCrimmon RJ. Clinical approaches to treat impaired awareness of hypoglycaemia. Ther Adv Endocrinol Metab 2021;12:20420188211000248.
- 3IHSG. A Blow to the Brain. Available at: https://staging.ihsgonline.com/2018/07/28/a-blow-to-the-brain/.
- 1Van Meijel LA et al. High prevalence of impaired awareness of hypoglycemia and severe hypoglycemia among people with insulin-treated type 2 diabetes: The Dutch Diabetes Pearl CohortBMJ Open Diabetes Res Care 2020;8:e000935.
- 2Farrell CM & McCrimmon RJ. Clinical approaches to treat impaired awareness of hypoglycaemia. Ther Adv Endocrinol Metab 2021;12:20420188211000248.
- 3IHSG. A Blow to the Brain. Available at: https://staging.ihsgonline.com/2018/07/28/a-blow-to-the-brain/.
How to treat moderate & severe hypoglycaemia (Levels 2 & 3)
Conscious person: Consuming 15–20 g of pure glucose is the preferred treatment, but any form of carbohydrates containing sucrose (such as candy, juice, or soft drink) may be used. If self-monitored blood glucose remains less than 4.0 mmol/L after 15 minutes, this treatment should be repeated.1
Unconscious person: Emergency services should be called and 1 mg of glucagon should be given subcutaneously (under the skin) or intramuscularly (in the muscle). In a hospital with intravenous (IV) access, 10–25 g of glucose should be administered IV.2
How to treat mild hypoglycaemia (Level 1)
Consume 15 g of fast-acting carbohydrates (such as juice or soft drink).2
Hypoglycaemia prevention strategies
References
- 1American Diabetes Association; 6. Glycemic Targets: Standards of Medical Care in Diabetes—2021. Diabetes Care 1 January 2021; 44 (Supplement_1): S73–S84.
- 2Diabetes Canada Clinical Practice Guidelines Expert Committee. Diabetes Canada 2018 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Can J Diabetes. 2018;42(Suppl 1):S1-S325
- 3Kreider KE et al. Practical Approaches to Diagnosing, Treating and Preventing Hypoglycemia in Diabetes. Diabetes Ther. 2017;8:1427–1435.
- 4Bhutani G et al. Effect of diabetic education on the knowledge, attitude and practices of diabetic patients towards prevention of hypoglycemia. Indian J Endocrinol Metab. 2015;19:383–386.
- 5Cho NH et al. Patient Understanding of Hypoglycemia in Tertiary Referral Centers. Diabetes Metab J. 2018;42:43–52.
What is glucagon?
Glucagon is a hormone that promotes the breakdown of glycogen to glucose, making it useful in raising blood glucose levels during a hypoglycaemic episode.
Types of glucagon
| Traditional glucagon kits1 |
FDA Approval 1988 with no age limitations Administration & Details
Recommended Dosage
|
| Nasal glucagon1 |
FDA Approval 2019 Administration & Details
Recommended Dosage
|
| Liquid-stable glucagon1 |
FDA Approval 2019 for paediatric and adult patients Administration & Details
Recommended Dosage
|
| Subcutaneous dasiglucagon2 |
FDA Approval 2021 Administration & Details
Recommended Dosage
|
| Glucagon Type | FDA Approval | Administration & Details | Recommended Dosage |
|---|---|---|---|
| Traditional glucagon kits1 | 1988 with no age limitations |
|
|
| Nasal glucagon1 | 2019 |
|
|
| Liquid-stable glucagon1 | 2019 for paediatric and adult patients |
|
|
| Subcutaneous dasiglucagon2 | 2021 |
|
|
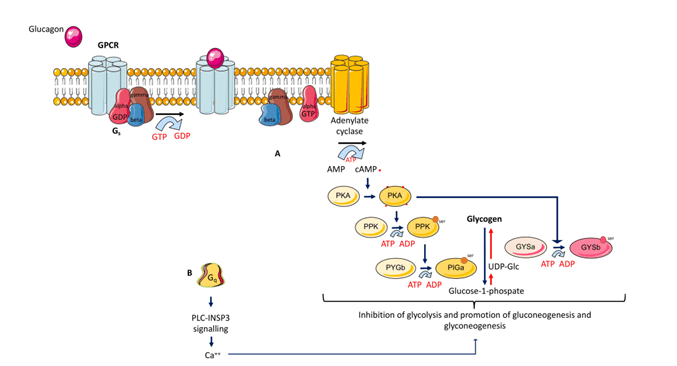
Mechanism of glucagon action, from La Sala & Pontiroli. 2021.2
Glucagon formulations undergoing clinical trials
Biochaperone glucagon3
- Recombinant human glucagon
- Prevents glucagon from degrading by adding compounds that form stable complexes with glucagon
Glucagon limitations
While useful, there are significant limitations to glucagon formulations. Glucagon formulations expire and are complicated to reconstitute. However, they are still used in many countries that don’t have access to nasal or pre-filled stable products.
References
- 1Sherman JJ, Lariccia JL. Glucagon Therapy: A Comparison of Current and Novel TreatmentsDiabetes Spectr. 2020;33:347–351.
- 2La Sala L & Pontiroli AE. New Fast Acting Glucagon for Recovery from Hypoglycemia, a Life-Threatening Situation: Nasal Powder and Injected Stable Solutions. 2021;22:10643.
- 3Beato-Vibora PI & Arroyo-Diez FJ. New uses and formulations of glucagon for hypoglycaemia. Drugs Context. 2019;8:212599.